Asthma is the most common chronic disease during the formative years and Alberta researchers are working on a project to improve the care for children affected by the respiratory condition.
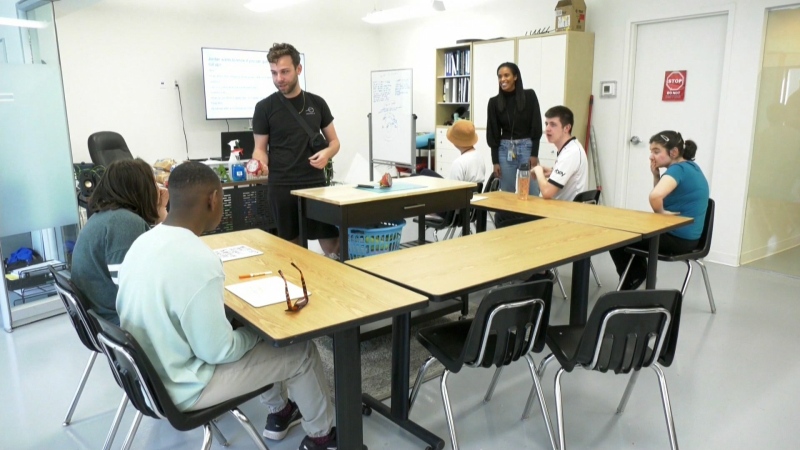
The project involves the development of an electronic care guide that family physicians and their staff can use to better manage the care they provide to asthma patients.
The treatment guide is put directly into the patient’s electronic medical record and the hope is that it will help to reduce the need for emergency department visits and hospital stays.
“What we’re attempting to improve is physician and parent management of asthma for their children,” said Dr. Andrew Cave, a family physician and Professor of Family Medicine at the University of Alberta. “So we developed a template that can be inserted into a patient’s electronic records for the doctor; they can click on it when a child with asthma comes through, and follow the path so the patient gets managed ideally.”
“So essentially what it is, is a series of questions posed to the physician to clarify, to help them really narrow down, to target in a really time efficient way, what type of asthma it is and then how best to treat it,” said Dr. David Johnson Professor of Paediatrics, Pharmacology and Physiology at the University of Calgary, Cumming School of Medicine.
The three-year study is being conducted at the U of C and U of A and is intended to assist health professionals to prescribe the right medication and to help parents fill and use the prescription properly.
“We’re hoping this intervention, this new initiative, will really help family physicians and parents to do a better job of managing their children’s asthma, thereby resulting in fewer emergency department visits and hospitalizations,” said Dr. Johnson. “Not all types of asthma are the same, there are sub-types of asthma and so they require different kinds of treatment, different kinds of approaches, and so because many family physicians, generalists, aren’t aware of that, it’s new information, they really need help to more efficiently manage kids to really ascertain what kind of sub-type it is and how to treat it.”
Other health professionals will also be trained to talk with parents and provide education on asthma treatments.
“By ensuring that family practitioners have a convenient tool that helps them provide the optimal therapy and by instructing the chronic-disease nurses in family practitioners’ offices on how to best educate parents to manage their kids with asthma, we offer the best chance to prevent kids from having to visit emergency or be hospitalized,” said Dr. Johnson.
Erin White’s son Noah has allergy-related asthma and uses inhalers and steroids.
“It’s really stressful, trying to remember, when was the last time he had this medication and the dosage and is he ready for this one and can he try something new and has he had a reaction to this and there’s all kinds of different triggers and it’s really stressful,” said White. “The idea that this is going to happen, we can type in his name, figure out exactly what he needs and when he needs it is going to be fantastic.”
“It can be kind of scary sometimes because I can’t really catch my breath and I start coughing really hard and I can’t catch my breath and I have to go in and get my medicine and then just stay inside,” said Noah. “I want to be able to get back outside and start playing again.”
The project is funded by a $750,000 grant and will be introduced by The Alberta Primary Care Pathway for Childhood Asthma to 22 medical practices in the province for a trial run.
If that is successful, researchers plan to roll it out province-wide.