Katie Flury was only 6-years-old when she lost her mother to breast cancer.
Now 29, and at a high-risk of facing the same diagnosis, Flury made a difficult choice.
She had a preventative double mastectomy and reconstruction. It would lower her chance of breast cancer to less than 1 percent.
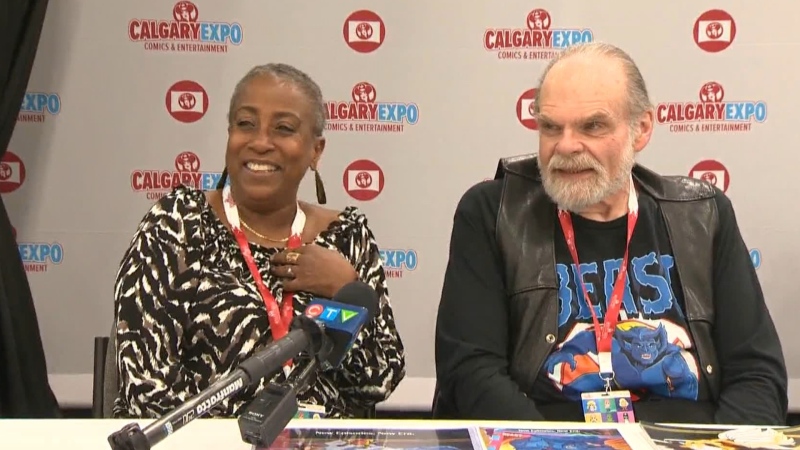
“For the average layperson, they might think it’s extreme,” says Dr. Walley Temple, a professor of surgery and oncology. “For the person that has this problem? No.”
Flury, like her mother, carries the faulty BRCA gene. Mutations on BRCA 1 and 2 genes have been associated with increased risk of breast and ovarian cancers. It’s the same condition actress Angelina Jolie disclosed publicly.
Flury learned she had an 87 percent chance of breast cancer, and a 60 percent chance of ovarian cancer.
Knowing her risk was higher meant regular breast exams, MRIs and mammograms. Constant testing was needed to make sure no cancer was developing.
“There was always the concern that could happen, and leave our kids without a mother,” says Katie’s husband, Mark Flury.
In early 2012, Flury began looking for other options and the next year, went under the knife.
The surgery took four hours. And while it was successful, her recovery process has been long and complicated.
“I kind of thought it would 4-6 weeks and then we’re good,” she explains. “But it’s been a lot longer than that.”
In the year since her first surgery, Flury has had multiple complications. She developed sores on her incision lines that lead to a strep infection.
“The one we really fear in implant reconstruction is infection,” explains Dr. Claire Temple-Oberle, Flury’s plastic surgeon. “Katie has had superficial infections which are easily treatable. But some women get them deep around their implant, and they lose the implant.”
Flury also developed cysts. They were taken out during a second surgery to revise her implants. Then she developed another similar infection, only this time it wasn’t contained to the stitches.
Then later this summer, the cysts returned.
“I knew obviously complications could happen. I had no idea this could happen. I’d never heard of it, I’ve never heard of anyone else having this,” she says.
Dr. Temple-Oberle says the complication is rare.
Alberta Health Services says 650 people are year are genetically tested in relation to breast cancer. Those who test positive for BRCA mutations have several different options. Some avoid surgery and continue close monitoring. Others have the preventative mastectomy, but choose not to have the reconstruction.
“It’s not for everybody,” says Dr. Temple-Oberle. “Some women have a mastectomy and they are very comfortable and they don’t want additional surgery or risk.”
Flury’s complications required a third surgery. The tissue around her implants was taken out, and replaced in an effort to stop more cysts from forming.
“I’m worried that this won’t fix it,” Flury says. “The last one, I had hopes everything would be good after that and it wasn’t.”
If the surgery isn’t successful, it could mean losing her implants and starting the reconstruction from scratch. She is willing to do that, but hasn’t decided if it would be immediate, or if she would wait. She will also have to decide on another drastic surgery down the line because her risk of ovarian cancer is also high.
“It’s terrifying for me,” she says. “It’s tough. I’m so thankful that I’ve had the opportunity to find out I have this gene, because my mom never did. There was nothing she could have done.”
Flury hopes she’s setting an example of courage for her son and daughter. Each has a 50 per cent chance of having the same gene mutation. She also hopes that if they ever test positive, there will be better options for protecting themselves than the surgeries she has had to endure.