A little bit pregnant: my journey from recurrent pregnancy loss to IVF
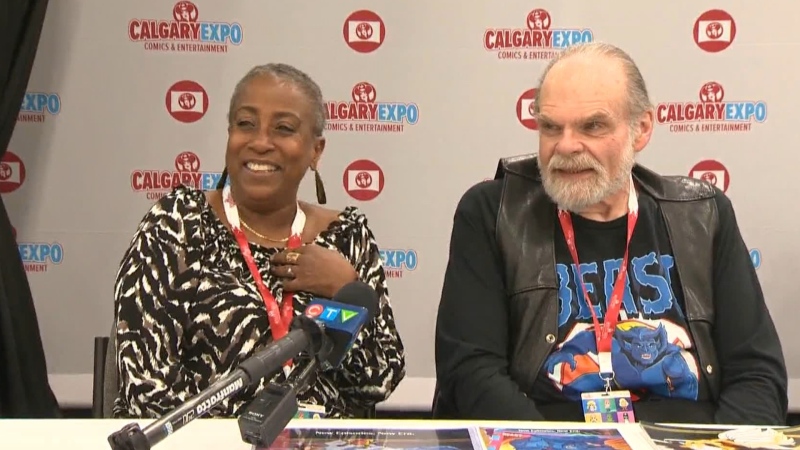
 Stephanie Thomas, CTV Calgary reporter
Stephanie Thomas, CTV Calgary reporter
Even the gorilla was pregnant, but I wasn’t. I was jealous of a zoo animal.
It’s understandable that trying to conceive can be so isolating, when it feels like social media feeds are full of black and white ultrasound images from happy couples announcing their news, it’s easy to feel left behind.
I was brought to tears while on assignment for a news story about an expectant gorilla at the Wilder Institute/Calgary Zoo as I interviewed patrons who were also mothers, many cradling round bellies. The pain I felt was so pervasive. I wanted to become a mother so badly.
The path to parenthood is challenging for an estimated one-in-six couples struggling with infertility according to the World Health Organization, but my struggle is a particular subset of that grim statistic. I could conceive, but I experienced recurrent pregnancy loss (RPL) without explanation. I felt blind-sided that this was even possible. I never met anyone who had gone through anything remotely similar.
UNEXPLAINED RECURRENT PREGNANCY LOSS
In less than three years, I’d had five positive pregnancy tests yet had four miscarriages. I’ll explain.
Three of my losses were similar. A few days after an expected period, I would take a test and see two pink lines indicating conception. Then about six to 10 days later, I would sense something going very wrong.
What happened next was both physically and emotionally overwhelming.
I went to urgent care the first time, but I’ve come to understand that there’s next to nothing to stop a miscarriage at around six-weeks-along. The other two times, I endured the agonizing process at home, while monitoring for any potentially life-threatening complications. Shame and self-doubt intensified each time.
One loss was particularly confusing. The pregnancy test showed a faint line on a Friday night, and again on Saturday morning, which was not a good sign. I waited hours for a blood test to confirm if the pregnancy hormone (beta-HCG) was high enough to indicate a healthy pregnancy.
By Sunday, I got my period.
By Monday, my gynaecologist confirmed, “You were pregnant, but not very pregnant.”
This is often called a biochemical pregnancy.
She also said, “I wish I had answers for you.”
EMOTIONAL TOLL, SEEKING ANSWERS
While less traumatic than my other experiences, I was in a drop-to-my-knees type of heartbreak over why this kept happening to us. It felt like I was riding a broken elevator that would rise just a little, but lower me back down to the lobby again, while seemingly everyone else was getting off at the ninth floor.
From the beginning I was on a mission for answers. I “triangulated” my care. My family doctor ordered tests and scans – as did my gynaecologist and fertility doctor. I knew I had to advocate for myself.
The resulting information was the same across the board. There were no barriers to conception and no explanations for the pregnancy losses.
No female factor issues were identified: no PCOS, no endometriosis, no problems ovulating, no anatomical challenges, no age-related concerns, no thyroid dysfunction, no auto-immune issues or any other health conditions that can affect pregnancy.
Critically, no male factor issues were ever found either.
WHAT COULD I DO?
The information I sought from reputable resources reflected what I was told by my own healthcare team: early pregnancy losses are often the result of an imbalance of chromosomes in the embryos.
It happens by chance and is often unexplained. It’s a random anomaly. It’s no one’s fault, they said.
Still, I blamed myself. Was I not thinking about it the right way? Was it a matter of lifestyle, or perhaps some environmental exposure? What could I do or not do?
I was avoiding perfume, nail polish and receipt paper among a list of things that can be considered harmful. Yet it didn’t seem to matter that I was also abstaining from alcohol and caffeine, taking expensive prenatal vitamins, doing yoga, acupuncture or hiking.
FINAL LOSS
Our final loss was the hardest, and it changed everything.
We made it to the eight-week ultrasound appointment, but the little baby was measuring only six weeks and three days. We saw a flickering heartbeat for the first time, and told some loved ones about the pregnancy thinking “surely, this is our time. This is our baby.”
A few days later on instinct, I went to the hospital to get checked out.
It was a bad sign when the emergency doctor walked me to an empty corridor to deliver the news from the ultrasound report. This baby was gone too.
I bawled, no howled, all the way home and immediately connected with the Pregnancy and Infant Loss Support Centre in Calgary. I was broken.
My husband and I knew we had to do something major if we wanted to build our family. Even though the fertility doctor said it would be reasonable to try again on our own, we made up our minds and wanted to do in vitro fertilization (IVF). He said he could treat us in a matter of weeks, but advised us to do extra pre-genetic testing (PGT-A) on the embryos we created to ensure the right balance of chromosomes.
I wanted to share my experience because I think anecdotes can be very powerful. I want anyone who may have a similar struggle to know there can be successful outcomes – and they aren’t alone. Also, assisted reproductive technology is often misunderstood and I assure you it isn’t a shortcut path to parenthood.
IDEAL IVF EXPERIENCE
The IVF process starts by stimulating the ovaries to produce more eggs in a cycle. Hormones are self-injected into the abdomen for several days before the mature eggs can be taken out in what’s called an egg-retrieval surgery. The eggs are immediately fertilized in the lab and embryologists monitor their development typically over five days.
In our case, we had 20 eggs retrieved, 17 fertilized right away, but seven embryos survived to the fifth day. Even with that dramatic drop-off, this is considered a great success as IVF can be “a numbers game.”
Just a few cells from those embryos were biopsied and shipped to a genetic testing centre in the USA. It found four of our embryos were chromosomally balanced! This meant we had four opportunities to achieve pregnancy with embryos that were likely to have the genetic information to become a healthy baby.
The next step is called a frozen embryo transfer (FET). In a quick appointment, one embryo was carefully placed inside my uterus. The embryologist explained it was graded high quality, and the procedure went off without any complications.
CONGRATULATIONS, YOU ARE PREGNANT
Just 12 days later, we got a phone call from the clinic: “Congratulations! You are pregnant! The expected due date is in February 2024.”
To have a positive pregnancy result after one IVF cycle followed by one FET cycle is the ideal scenario. Every single day of my pregnancy was filled with gratitude for such a quick progression. It also helped erase my feelings of failure. After repeated devastation, this fertility treatment finally restored my hope.
 CTV Calgary reporter Stephanie Thomas seen here with her new daughter Evelyn Rhea Thomas. (Photo courtesy Stephanie Thomas)
CTV Calgary reporter Stephanie Thomas seen here with her new daughter Evelyn Rhea Thomas. (Photo courtesy Stephanie Thomas)
TURNING PAIN INTO PURPOSE
As a journalist, I often meet families after tragedy as they turn their “pain into purpose.” They become advocates in hopes to help others avoid similar pain. It helps with their healing. They also press for better research, more answers, and often get results.
So I hope I can do the same by sharing our story. Reproductive science and medicine has a long way to go to address why recurrent pregnancy loss most often goes unexplained. While I’m at peace with our past, to be “just unlucky” is not good enough. No one else should go through what we went through.
However, I want to share our positive experience with assisted reproductive technology and IVF for others who may wind up at a fertility treatment centre. It required diligence, plenty of trust in multiple medical professionals along the way, all at a large out-of-pocket expense.
But it was so worth it. We were on our way to becoming parents. I’d ached to become a mother for so long. I was overjoyed at every positive scan or appointment during the pregnancy and nothing felt routine.
Just a short time ago, when we weren’t sure if it would ever happen for us.
Now we are facing a beautiful new reality that it’s finally our time.
Editor’s note: On Feb. 18, 2024 Evelyn Rhea Thomas was born at 10:07 a.m. A happy coincidence on Alberta’s Family Day Long Weekend.
---
As journalists, we often come across a story, person, place or situation that leaves a lasting impression and we wish we could share more with our viewers than the 90 seconds television allows.
Postscript gives us a place to present those little extras and dig a little deeper into those stories that most interest Albertans.
We are pleased to share the more memorable moments from some of our most experienced reporters and anchors with our viewers.
CTVNews.ca Top Stories

More than 115 cases of eye damage reported in Ontario after solar eclipse
More than 115 people who viewed the solar eclipse in Ontario earlier this month experienced eye damage after the event, according to eye doctors in the province.
Toxic testing standoff: Family leaves house over air quality
A Sherwood Park family says their new house is uninhabitable. The McNaughton's say they were forced to leave the house after living there for only a week because contaminants inside made it difficult to breathe.
Decoy bear used to catch man who illegally killed a grizzly, B.C. conservation officers say
A man has been handed a lengthy hunting ban and fined thousands of dollars for illegally killing a grizzly bear, B.C. conservation officers say.
B.C. seeks ban on public drug use, dialing back decriminalization
The B.C. NDP has asked the federal government to recriminalize public drug use, marking a major shift in the province's approach to addressing the deadly overdose crisis.
OPP responds to apparent video of officer supporting anti-Trudeau government protestors
The Ontario Provincial Police (OPP) says it's investigating an interaction between a uniformed officer and anti-Trudeau government protestors after a video circulated on social media.
An emergency slide falls off a Delta Air Lines plane, forcing pilots to return to JFK in New York
An emergency slide fell off a Delta Air Lines jetliner shortly after takeoff Friday from New York, and pilots who felt a vibration in the plane circled back to land safely at JFK Airport.
Sophie Gregoire Trudeau on navigating post-political life, co-parenting and freedom
Sophie Gregoire Trudeau says there is 'still so much love' between her and Prime Minister Justin Trudeau, as they navigate their post-separation relationship co-parenting their three children.
Last letters of pioneering climber who died on Everest reveal dark side of mountaineering
George Mallory is renowned for being one of the first British mountaineers to attempt to scale the dizzying heights of Mount Everest during the 1920s. Nearly a century later, newly digitized letters shed light on Mallory’s hopes and fears about ascending Everest.
Loud boom in Hamilton caused by propane tank, police say
A loud explosion was heard across Hamilton on Friday after a propane tank was accidentally destroyed and detonated at a local scrap metal yard, police say.